From the CEO: Democracy Depends on Courage

Democracy at Work in Guyana: A Pivotal Election Day

Guinea Worms Live on Borrowed Time in Ethiopia

Carter Center Launches New Website
Mental Health Care Transformation

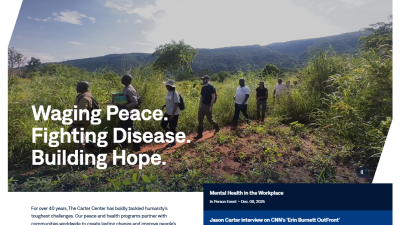
Waging Peace: A Legacy

Documentary Debut: The President and The Dragon

The Last Focus

In Bangladesh, USAID Cuts Force Women’s Program to ‘Reimagine What’s Possible’

In Rule of Law, Director Seeks Fairness for All

1 of 44
Global Impact Starts with You
Your support sustains the Carter Center's mission of waging peace, fighting disease, and building hope around the world.




